Introduction:
Newer treatments have permitted more older patients with acute myeloid leukemia (AML), including those with aging-related conditions, to receive leukemia-directed therapy. A better understanding of patient values (i.e., their priorities) as well as informational and decisional preferences is important to achieve high-quality shared decision making. In this study, we 1) describe the values of older adults with newly diagnosed AML; 2) assess demographics and aging-related conditions associated with patient values; and 3) describe informational and decisional preferences.
Methods:
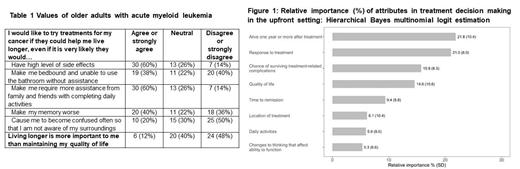
We combined data from two studies: a single arm pilot (UR-GOAL 1) and a pilot randomized controlled trial (UR-GOAL 2) testing a communication tool among adults aged 60 and over with newly diagnosed AML. Caregivers were also recruited when available. Patients completed questionnaires on personal values as well as informational and decisional preferences. The value questionnaire asked patients to consider trade-offs between survival and two clinical outcomes: a) maintaining quality of life (QoL) and b) five specific treatment-related toxicities (nausea/vomiting, bedbound status, assistance with daily activities, worsening memory, confusion; Table 1). Best-Worst Scaling (BWS), where participants complete choice tasks identifying most and least important attributes (i.e., factors that are important to individuals), was used to elicit the relative importance of each attribute to patients. We used descriptive analyses to summarize patient values and informational and decisional preferences. We used Hierarchical Bayes multinomial logit modeling to estimate the importance of attributes for the BWS. Generalized linear regression models were used to assess demographics and aging-related conditions associated with patient values.
Results:
We included 50 patients; mean age was 74.1 (SD 7.9), 66% were male, 94% were White, and 48% enrolled with a caregiver. Table 1 shows the responses on trade-offs between survival and clinical outcomes. Only 12% agreed or strongly agreed that living longer was more important than maintaining QoL. Fifth-percent reported that they would not like to try treatments if they would cause them to become confused and 40% would not like to try treatments if they would make them bedbound. The relative importance of the 8 attributes from the BWS instrument are shown in Figure 2 (order of importance: survival, response to treatment, treatment-related death, QoL, time to remission, location of treatment, daily activities, cognition).
On multivariate analyses, younger patients (every 10-year increase in age; B=-1.19, p<0.01) and those enrolled with caregivers (B=1.76, p<0.01) were more likely to accept a trade of treatment-related toxicities for survival. Male patients (B=0.91, p=0.06) and those without nutritional impairment (B=1.38, p=0.05) may also be more likely to accept a trade of treatment-related toxicities for survival. On multivariable analysis using data from the BWS instrument, younger patients (every 10-year increase in age; B=-6.57, p=0.07) may be more likely to prioritize attributes such as survival and remission over attributes such as QoL, cognition, and daily activities.
In terms of informational preferences, 76% preferred information about treatment success rate to be presented in percentages, 52% preferred to hear about previous patients that their doctors had treated, 24% preferred words, and 22% preferred fractions.
For decisional preferences, 46% preferred to share equally in decisions about their care with their doctor, 28% preferred to make medical decisions with significant input from their doctor, 18% preferred to have their doctor make decisions with significant input from them, and 8% preferred to leave their care and treatment to their doctor. No one preferred to be the one making decisions about their medical care.
Conclusions:
Values as well as informational and decisional preferences are heterogeneous among older adults with AML, and they should be elicited as part of standard shared decision making to personalize management recommendations. Younger patients and those enrolled with caregivers were more likely to prioritize survival over treatment-related toxicities when choosing treatments. Novel interventions are needed to capture values and preferences in real-time to achieve high-quality shared decision making.
Disclosures
Loh:Pfizer: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal